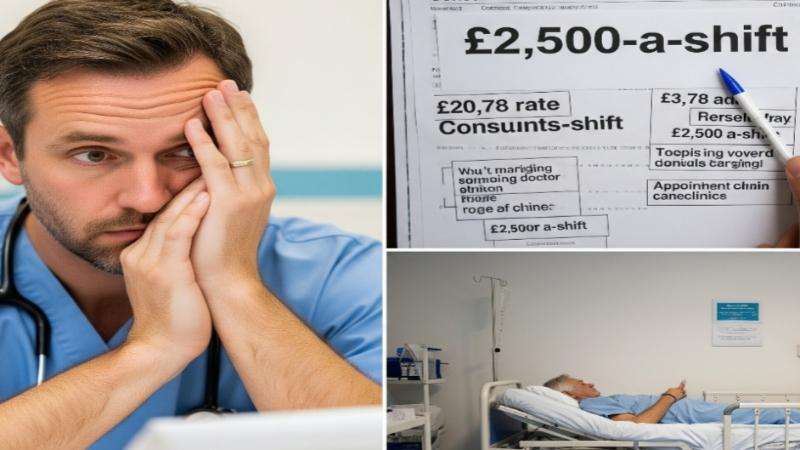
NHS consultants are facing accusations of exploiting the ongoing junior doctor strikes by allegedly cancelling their own patient clinics and operating lists, only to then charge the health service astronomical fees — up to £2,504 for a single eight-hour overnight shift — to cover the very gaps they've helped create. This explosive claim adds a new, controversial dimension to the already protracted industrial dispute, raising serious questions about patient welfare and the integrity of the healthcare system.
The fees, branded "outrageous" by senior medics, are based on the British Medical Association's (BMA) 2025 consultant extra-contractual rate card. These figures reveal that during periods of industrial action:
Weekday day shifts (7 am–7 pm) are charged at £188 an hour.
Weekend shifts are billed at £250 an hour.
Overnight shifts (11 pm–7 am) soar to £313 an hour.
On-call cover, even if no work is performed, is charged at £125 an hour.
This means a consultant could claim £2,504 for one overnight shift, in addition to their regular full-time NHS salary, with the cost ultimately borne by the taxpayer.
"Having Their Cake and Eating It"
A senior NHS consultant and advisor, who spoke anonymously to GB News, revealed the alarming extent of the alleged practice. "The BMA rates are extortionate – but consultants are having their cake and eating it. They are deliberately cancelling their own clinics and operating lists in support of the strikes, then charging huge amounts to cover for the striking junior doctors."
This alleged deliberate cancellation of scheduled NHS work, including cancer operations and chemotherapy clinics, is reportedly designed to amplify the impact of junior doctor strikes. "This is an unwritten and unofficial deal between the junior doctors and consultants. If they didn’t stand down their own work, the strike action would have far less impact,” the source added.
Junior doctors primarily handle ward rounds and routine tasks, meaning their direct impact on waiting lists is somewhat limited. However, with consultants stepping back, the disruption is significantly magnified, leading to potentially critical delays in patient care. "It’s happening up and down the country. I’ve expressed my opposition to colleagues – and they just laugh at me," the anonymous consultant lamented.
Worsening NHS Crisis and Patient Backlog
The revelations come as the NHS continues to grapple with an unprecedented backlog. More than 40 strike days have occurred since 2022, severely impacting services and exacerbating pressure on an already stretched healthcare system. Data analysis by health consultancy Broadstone recently warned that ongoing strike action will add hundreds of thousands of patients to NHS waiting lists, particularly those requiring planned operations and specialist care.
A former NHS executive condemned the situation, stating, "These new figures expose just how warped the system has become. We now have senior doctors cancelling their own work, costing the NHS twice – once in lost care and again in inflated strike cover fees.”
BMA Responds, Government Stance
The BMA declined to comment directly on the allegations that consultants were deliberately cancelling clinics. It stated that the ‘extra-contractual pay rates’ are to cover for any additional work, not solely resident doctor strikes.
Meanwhile, Dr. Melissa Ryan and Dr. Ross Nieuwoudt, co-chairs of the Resident Doctors Committee, reiterated their position on negotiations. They stated that they met with Wes Streeting, the Shadow Secretary of State for Health and Social Care, and attempted to open negotiations for pay restoration to avoid further strike action. However, they claim the Government has refused to negotiate on pay, choosing instead to focus on "non-pay elements" without specifying what these might be.
"Without a credible offer to keep us on the path to restore our pay, we have no choice but to call strikes," they stated, adding, "No doctor wants to strike, and these strikes don’t have to go ahead. If Mr Streeting can seriously come to the table in the next two weeks we can ensure that no disruption is caused. The Government knows what is needed to avert strikes. The choice is theirs.”
The BMA's latest strike mandate remains valid until January 2026, meaning further significant disruption looms if a resolution is not reached.
Ethical Concerns and Calls for Action
Concerns are mounting over the ethical implications of the alleged practices. One NHS advisor, a senior consultant who wished to remain anonymous, questioned the Hippocratic Oath, stating, "Do these doctors not follow their Hippocratic Oath - first do no harm? These strikes will lead to the cancellation of operations worsening the NHS waiting lists. It will also lead to the cancellation of vital appointments leading to treatments and operations. This includes lifesaving interventions such as chemotherapy and surgery for cancer. This could cost lives. It is messing up the NHS at a time when it is starting to show slow signs of recovery.”
Professor Carl Heneghan, an urgent care GP and director of Oxford University’s Centre of Evidence Based Medicine, called the situation a "national emergency." He urged for a focus on getting patients in front of doctors, especially for cancer diagnosis and treatment, advocating for stripping out unnecessary agencies and prioritizing direct patient care over unproven technological solutions.
Daniel Elkeles, Chief Executive of NHS Providers, expressed strong disapproval, stating that "Announcing five days of strike action with just two weeks’ notice can only be harmful. It’s totally unfair to patients whose care will be cancelled at such short notice just as the NHS was beginning to turn the tide on reducing waiting lists.” He emphasized the need for "cool heads to de-escalate this and remove the threat of further damaging industrial action."
Wes Streeting has also voiced his strong disapproval of the ongoing strikes, stating last week, “The public will not forgive strike action in these circumstances and nor will I.” In a letter to the BMA, he added, “By choosing to strike instead of working in partnership to improve conditions for your members and the NHS, you are squandering an opportunity.”
The number of patients waiting over a year for treatment recently increased for the second consecutive month, now standing at 196,000. Meghana Pandit, Co-National Medical Director for NHS England, acknowledged doctors' frustrations but stressed that "industrial action comes at a significant cost to patients and frontline colleagues, and they will rightly expect steps are taken to avoid strikes from going ahead.”
The escalating dispute, coupled with these new allegations, casts a shadow over the future of NHS patient care and the ethical conduct of some within the medical profession.
What are your thoughts on these new allegations against consultants, and how do you think they might impact public perception of the ongoing industrial action?

_4.jpg)




.svg)

.jpg)
